Treatment: Radiation therapy
Radiation therapy (radiotherapy) of Dupuytren’s and Ledderhose Disease
Radiation therapy (radiotherapy) is a non-surgical treatment that can stop or slow down Dupuytren’s disease in its early stage. In radiation therapy, the nodules and cords associated with Dupuytren’s are irradiated from a distance of .5 – 1 cm either with X-Rays (e.g. 120 kV) or with electrons (3 – 10 MeV). This is typically done over five days in a row applying an efficient dose (single dose 3 Gy, total dose 15 Gy). After a break of 6 -12 weeks, this treatment is repeated. Typically this softens the nodules (and somtimes also cords) and prevents contraction of the hand. Recently research showed that a total dose of 20 Gy has nearly the same effect (see literature).
An expert diagnosis prior to radiotherapy is important!
Prior to radiotherapy the to be irradiated area has to be defined by the physician. Because RT is usually not repeated it is very important that all sites of Dupuytren’s in the hand are identified and included within the irradiated area. At the same time not diseased areas are usually not irradiated to minimize risk of cancer and to allow later treatment in case DD should start in those areas. MRIs are rarely required for diagnosis but an experienced physician will be able to palpate even tiny nodules and cords. Below picture illustrates the difference between a patients finding (left) the result of the physician’s palpation (right).
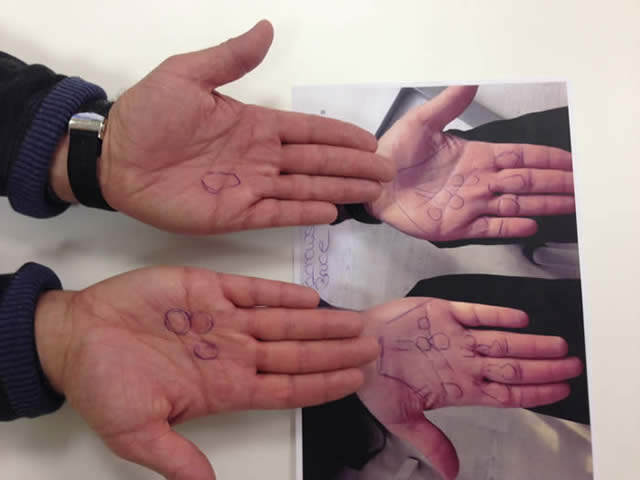
Nodules and cords identified by the patient (left) and the additional findings of the physician (right).
(Picture published with agreement by the patient and H. Seegenschmiedt, Strahlenzentrum Hamburg Nord, Germany)
Where radiotherapists have limited experience in diagnosing Dupuytren’s it might be feasible to consult an experienced hand surgeon for marking the nodules.
Therapy pictures:
E-beam:
 |  |
| The irradiated area is marked on the hand. | The hand is ready for treatment. Note that there is no shielding required. |
X-ray:

Setup for radiation therapy of Dupuytren’s disease (Dupuytrens) with X-rays. The patient is shielded from radiation by the equipment itself, by a lead mask between the x-ray conus and the hand (defining the radiated area), the material under the hand, and the lead apron.
(Picture provided by H. Seegenschmiedt, Strahlenzentrum Hamburg Nord, Germany)
Positive effects of radiotherapy
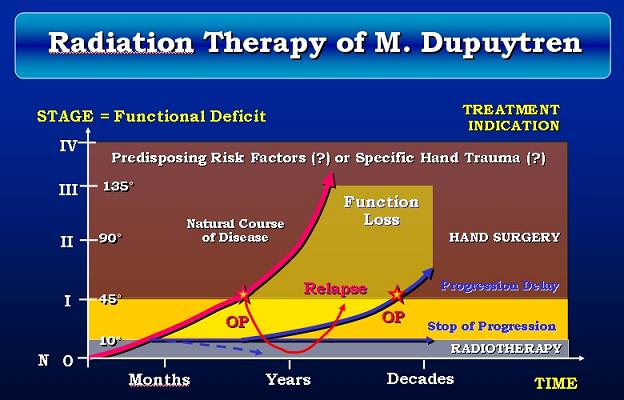
Radiotherapy is capable of stopping the growth of Dupuytren nodules either permanently or for a long time. Occasionally, small nodules will even shrink or disappear. Radiotherapy is much less effective on cords and cannot make an already bent finger straight again. Below is a graph from a presentation by Seegenschmiedt et al. at the ASSH meeting 2006 illustrating how radiation therapy delays disease progression and in favorable cases can render surgery unneccessary. Blue lines indicate the disease progression after radiotherapy, the dotted line indicates a potential healing effect in early stage treatment (for details please refer to the full presentation).
Radiotherapy – when to apply best?
The effectiveness of radiotherapy depends on the stage of the disease. It is very promising in the early nodular stage where the nodules are relatively small. Research at the University of Erlangen, Germany, showed the following: ten years after the therapy, for 84 percent of the patients having Dupuytren in stage N (just nodules and cords) and 67 percent of stage N/I (hand bent by 1-5°), the disease either had not progressed or had actually improved (Adamietz et al. „Radiotherapy in Early Stage Dupuytren’s Contracture“, see literature). The success rate becomes much lower in later stages. Overall, radiation therapy seems to be able to stop or significantly slow down Dupuytren’s disease in the early stage. If it doesn’t, surgery, NA or collagenase injection are still possible.
Long-term results from Betz et al. („Radiotherapy in Early Stage Dupuytren’s Contracture – Long Term results after 13 Years“ 2010 literature) clearly demonstrate the advantage of early treatment. It is most effective to treat the Dupuytren’s nodule within the first year, probably best as soon as possible (status idem = stable, no change):
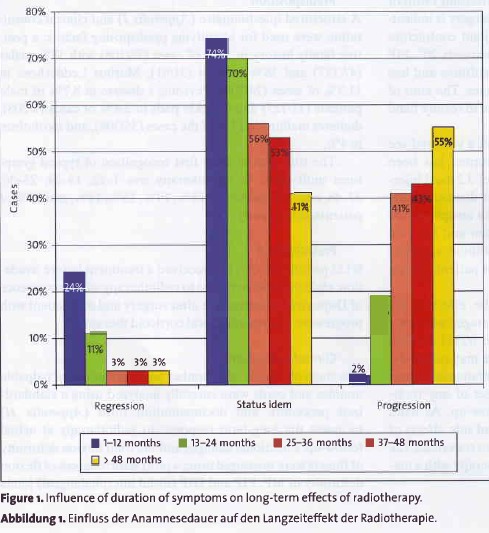
One of the difficulties of radiation treatment is that only a few people consult their doctor in the very early stage of Dupuytren’s, when the nodules are only a few millimeters in diameter and when radiation treatment is most beneficial. Another problem is that radiotherapy as a means for treating Dupuytren’s disease is not widely known.
Who should be treated?
It is important to understand that not every patient with Dupuytren’s nodules will experience contracture. Seegenschmiedt et al. abstract compared patients treated with radiotherapy (21 and 30 Gy) and an untreated control group with an average follow-up of 8 years. In that period the extension deficit increased for 35% of the patients in the untreated group and in 7% (21 Gy) and 4% (30 Gy), respectively, in the treated groups. But that also means that over 8 years of observation 2/3 of the untreated patients experienced no increase of their extension deficit. People who develop initial signs of Dupuytren’s at the age of 70 or later will often not need treatment at all. Prevalence considerations indicate that the percentage of people with symptoms of Dupuytren disease who never need any kind of treatment, maybe even be higher, up to 85%.
Clear guidelines for who should be treated by radiotherapy and who not are still missing. Treatment by radiotherapy probably makes sense for patients with aggressive Dupuytren’s where RT can slow down or halt disease progression and who otherwise would have to face later surgery or frequent minimally invasive treatments. The aggressiveness of Dupuytren’s disease may depend on several factors, one of them being age. Patients with a dormant disease or low probability for recurrence might get along well with a „wait and see“ strategy. As radiotherapy of Dupuytren and Ledderhose disease often also relieves pain, patients suffering from painful disease might also be potential candidates for radiotherapy.
Additional detailed consideration and information on radiotherapy (specifically at a Hamburg clinic) are provided by a patient (Alastair Cook) on dupuytrensradiotherapy.
Radiation therapy – how does it work?
Dupuytren’s disease and Ledderhose disease start with fibrous tissue in form of nodules that, specifically in its initial stage, is biologically very active („proliferative“). Like in wound healing this tissue maturates (building cords for Dupuytren’s) and eventually contracts (actively or passively fixing a contraction). The initial proliferating stage is most suitable for radiotherapy. Radiotherapy seems to be able to affect the development of the involved fibroblast and myofibroblast cells (in other terms the involved growth factors) and reduce their growth rate. There is indication that this is achieved by affecting the development paths of the myofibroblast cells. As the growth of a nodule is the net effect of building new cells and of removing dead cells, the slowing down of the growth of new cells can result in shrinking and softening of the nodule. – While there is a variety of publications on the macroscopic results of radiotherapy of Dupuytren’s, the understanding of the radiobiological proccesses is still a matter of basic research. For more details please refer to „Introduction to radiation biology when treating hyperproliferative benign diseases“ link , or literature (section 9.5.3.1. of „Radiotherapy for Non-Malignant Disorders“, and the Degro 07 paper by Blaese and Rodemann).
Further questions and answers
Questions by patients have been discussed in our forum and you might find below answers interesting (mostly by Prof. Heinrich Seegenschmiedt from Essen, Germany).
Definition of Dupuytren’s Disease progression
Clinical examination of Dupuytren’s prior to RT
Treatment of DD after RT (re-radiation)
Radiotherapy of Ledderhose disease
Above comments apply for Ledderhose accordingly. Because Ledderhose shows less cords but mostly larger nodules, radiation therapy is applied to those larger nodules as well. Below is an example of an x-ray treatment showing how lead shielding is applied for limiting the radiated area (shielding of electron beams is more difficult, therefore typically the whole area is radiated). Below pictures were provided by Dr. Herkströter of Städtische Kliniken Frankfurt.

Marking of nodule (dotted, center) and to be radiated area prior to treatment.

Protecting the surrounding area with a lead shield prior to x-ray treatment.

Treatment position. X-ray equipment applied.
(pictures provided by Städtische Kliniken Frankfurt/M.-Höchst)
Example of treatment results, provided by a patient:

Before radiotherapy the nodule or nodules extend over a large area of the arch.

After radiotherapy the nodule is not gone but reduced in size.
Patient’s comment: „I’m really satisfied about my condition nowadays. Even the walking difficulties and pain got much better.“
Page last modified: 01/03/2025
